Merkel Cell Carcinoma Warning Signs
What You Need to Know
Merkel cell carcinoma (MCC) is rare and dangerous but treatable, especially when found at an early stage. Be watchful for any new or changing lesions on your skin and look out for these warning signs.
If you’ve been treated for a previous MCC, pay close attention to the site and the surrounding region. Contact your medical team immediately if you see any suspicious changes.
How to spot a Merkel Cell Carcinoma
APPEARANCE
Painless shiny or pearly lesions or nodules
SIZE
Dimensions vary, but the average size at detection is 1.7 cm, about the diameter of a dime.
COLOR
Skin-colored, red, purple or bluish-red
LOCATION
Frequently on sun-exposed areas, often on the head and neck, particularly the eyelids.
While rare, Merkel cell carcinomas are often aggressive and can advance rapidly which is why early detection and removal are especially important. Memorial Sloan Kettering oncologist Sandra D’Angelo, MD, shares some important warning signs you should never ignore.
Risk factors + warning signs = AEIOU
Since MCCs can progress rapidly and become more difficult to treat, it’s crucial to understand your risks and warning signs. This AEIOU summary combines key points from both to help you with early detection.
- A: ASYMPTOMATIC lesion, not painful or tender
- E: Lesion is EXPANDING rapidly
- I: You are IMMUNOsuppressed
- O: You are OLDER than 50
- U: The lesion appears on UV-exposed skin
In a study of 195 patients, 89 percent of MCC patients presented with three or more of the “AEIOU” characteristics.
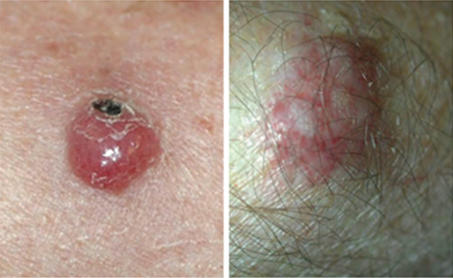
Left photo: Merkel cell carcinoma, local recurrence, forehead
Right photo: Merkel cell carcinoma, primary tumor, lower arm
Photos courtesy of Paul Nghiem, MD, PhD
Please note: Since not all MCCs have the same appearance, these pictures of Merkel cell carcinoma serve as a general reference for what MCC can look like. If you see anything NEW, CHANGING or UNUSUAL on your skin, go get checked by a dermatologist.

Merkel cell carcinoma on woman’s left eyelid.

Merkel cell carcinoma on arm. Photos courtesy of Paul Nghiem, MD, PhD
Challenges in diagnosis
Diagnosis and management of Merkel cell carcinoma presents distinct challenges, including:
- Misdiagnosis: 56 percent of MCCs are believed to be benign when initially examined by physicians, who may mistake the tumors for cysts or infected hair follicles.
- Delayed medical attention: Medical care is often not sought early as these lesions do not appear concerning. About 5 percent of MCCs occur in mucosal sites such as the mouth, nasal cavity and throat, where these painless lesions are hard to spot before the disease has advanced.
- Undetectable: In one study, 14 percent of MCCs were initially discovered in the lymph nodes already, without any tumor being identified.
Since MCC is a rare and aggressive cancer, delayed detection, diagnosis and treatment are especially concerning, because as the disease progresses, treatment becomes more difficult and the risk of recurrence increases.
What you can do
- Examine your skin head-to-toe every month.
- See your dermatologist every year for a professional skin exam. If you are newly diagnosed with MCC, seek a consultation with a multidisciplinary expert. Find a specialist here.
- If you’ve had an MCC, follow up regularly with your dermatologist once treatment is complete. Follow the exam schedule your doctor recommends — it’s the best way to quickly detect a recurrence. Consider getting the AMERK biomarker blood test that can help detect recurrences early. Learn more here.
- Safeguard your skin and avoid unprotected UV exposure. It is the single most effective way to reduce your risk of developing MCC.
- Practice sun-safe habits, such as seeking shade and wearing protective clothing, a wide-brimmed hat and UV-blocking sunglasses. Use a broad-spectrum sunscreen every day. Sunscreen is a good defense against premature aging and skin cancer. It’s never too late to start wearing it!
Reviewed by:
Sandra D’Angelo, MD
Paul Nghiem, MD, PhD
Last updated: August 2022




