Squamous Cell Carcinoma Treatment
Effective Treatment Options for Early Stage SCC
Most squamous cell carcinomas (SCCs) of the skin can be cured when found and treated early. Treatment should happen as soon as possible after diagnosis, since more advanced SCCs of the skin are more difficult to treat and can become dangerous, spreading to local lymph nodes, distant tissues and organs. Find out more about treatment options for advanced or recurring SCCs here.
If you’ve been diagnosed with an SCC that has not spread (in situ), there are several effective treatments that can usually be performed on an outpatient basis. The choices available to you depend on the tumor type, size, location and depth, as well as your age and overall health.
Options include:
- Excisional surgery
- Mohs surgery
- Cryosurgery
- Curettage and electrodesiccation (electrosurgery)
- Laser surgery
- Radiation
- Photodynamic therapy (PDT)
- Topical medications
- Immunotherapy
Ask your dermatologist to clearly explain the options that might work best for you, including details about the risks and benefits. Check our treatment glossary for more detailed information.
Excisional surgery
How it works
Using a scalpel, the surgeon removes the entire tumor along with a “safety margin” of surrounding normal tissue. The margin of normal skin removed depends on the thickness and location of the tumor.
Typically, the patient goes home after the surgery, and the excised tumor goes to the lab. If the lab finds cancer cells beyond the margins, the patient may need to return for more surgery until margins are cancer-free.
When it’s used
For small, early SCCs that have not spread, excisional surgery is frequently the only treatment required.
Mohs surgery
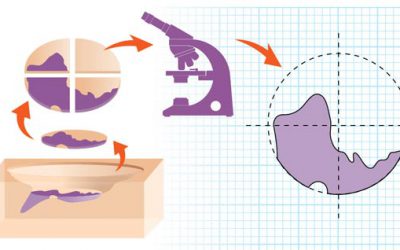
How it works
Mohs surgery is performed during a single visit, in stages. The surgeon removes the visible tumor and a very small margin of tissue around and beneath the tumor site. The surgeon color-codes the tissue and draws a map correlated to the patient’s surgical site. In an on-site lab, the surgeon examines the tissue under a microscope to see if any cancer cells remain. If so, the surgeon returns to the patient and removes more tissue exactly where the cancer cells are. The doctor repeats this process until there is no evidence of cancer. Then the wound may be closed or, in some cases, allowed to heal on its own.
When it’s used
Mohs surgery is the most effective technique for removing SCCs, sparing the greatest amount of healthy tissue while achieving the highest possible cure rate – up to 97 percent for tumors treated for the first time. It is often recommended for SCCs located in small, cosmetically or functionally important areas around the eyes, nose, lips, ears, scalp, fingers, toes or genitals. Mohs is also used for SCCs that have recurred, and for tumors that are large or growing rapidly, as well as ones with indistinct edges. Learn if Mohs is right for you.
Superficial versus minimally invasive
Superficial SCCs have not penetrated (or invaded) below the topmost layer of the skin (the epidermis), while minimally invasive SCCs have just barely invaded the second layer of skin (the dermis) and have no high-risk characteristics.
Curettage and electrodesiccation (electrosurgery)
How it works
The physician scrapes or shaves off the SCC with a curette (a sharp instrument with a ring-shaped tip), then uses heat or a chemical agent to stop the bleeding and destroy remaining cancer cells. The procedure may be repeated a few times during the same session until no cancer cells remain.
When it’s used
Curettage and electrodesiccation can be effective for most small, superficial or minimally invasive SCCs.
Cryosurgery
How it works
The physician uses a cotton-tipped applicator or spray device to apply liquid nitrogen to freeze and destroy the tumor, which eventually falls off, allowing healthy skin to emerge.
When it’s used
Cryosurgery is effective for superficial SCCs, especially for patients with bleeding disorders, implantable cardiac devices or problems tolerating anesthesia.
Laser surgery
How it works
The physician directs a beam of intense light at the tumor to target the cancerous cells. Some lasers vaporize (ablate) the skin cancer, while others (nonablative lasers) convert the beam of light to heat, which destroys the tumor.
When it’s used
Laser surgery is not yet FDA-approved for SCC but is sometimes used for superficial SCCs, especially when other techniques have been unsuccessful.
Radiation
How it works
The physician uses low-energy X-ray beams to destroy the tumor, with no need for cutting or anesthesia. Destruction of the tumor may require several treatments over a few weeks or daily treatments for a specified time.
When it’s used
Radiation therapy is primarily used for SCCs that are hard to treat surgically, and in elderly patients or people in poor health for whom surgery is not advised. For some cases of advanced SCC, especially those with perineural involvement, radiation may be used after surgery, or in combination with other treatments.
Photodynamic therapy (PDT)
How it works
The physician applies a light-sensitizing topical agent and, after allowing a period of time for absorption, directs a strong red or blue light or a pulsed-dye laser at the tumor to activate the topical agent, killing cancer cells while sparing healthy tissue. After the procedure, patients must strictly avoid sunlight and indoor tanning for at least 48 hours, as ultraviolet exposure will increase activation of the medication and may cause severe sunburns.
When it’s used
PDT can be used for some superficial SCCs on the face and scalp but is not recommended for invasive SCCs. It is most effective for treating actinic keratoses, which can be precursor lesions to SCC.
Topical medications
How it works
5-fluorouracil (5-FU) and imiquimod are creams or gels that can be applied directly to affected areas of the skin to treat superficial SCCs with minimal risk of scarring. Imiquimod activates the immune system to attack cancerous cells, while 5-FU is a topical therapy that targets cancerous and precancerous cells.
When it’s used
While these topical medications are not yet FDA-approved for treating SCCs, they are sometimes used for superficial tumors. The medications are also used preventatively for AKs.
Treating advanced SCCs
More extensive treatment is necessary for SCCs that have spread, are large in size, have penetrated the skin deeply and caused severe local damage or have resisted multiple treatments and recurred. Find out more about these treatment options here.
Immunotherapy
Immunotherapies boost the immune system’s ability to fight disease. Cemiplimab (Libtayo®) is an intravenously infused anti-PD-1 immune checkpoint inhibitor that works by inhibiting a protein receptor called PD-1 that normally blocks the immune system. This allows T cells to be released to fight the cancer. This treatment has been FDA-approved since 2018 for locally advanced or metastatic SCC of the skin.
However, in October 2025, the FDA also approved cemiplimab as the first immunotherapy for adjuvant treatment of cutaneous squamous cell carcinoma (SCC) of the skin that has a high risk of recurrence after surgery and radiation. This is the first FDA approval of this type of treatment for some patients with earlier SCC that has not advanced.
The approval was based on data from a clinical trial investigating adjuvant cemiplimab versus placebo in patients with cSCC at high risk of recurrence after surgery and radiation. Results from the study, which were published in the New England Journal of Medicine, showed a 68 percent reduction in the risk of disease recurrence or death compared with placebo in patients with cSCC at high risk of recurrence after surgery and radiation.
Reviewed by:
Elizabeth K. Hale, MD
C. William Hanke, MD
Note: The information included on this website is medically reviewed and factually accurate. It is intended for educational purposes only. The treatment information on this page is not a recommendation or endorsement of any drug, device or treatment, nor does it suggest that any drug, device or treatment is safe or effective for you. If you have any questions about skin cancer treatments, please talk to your health care provider.


