Photo: MORSA IMAGES/DIGITALVISION/GETTY IMAGES
Among the millions of people diagnosed with basal cell carcinoma (BCC) each year, most are easily treated, but some are not so lucky. Our experts explain how BCC can become advanced and, in rare cases, even life-threatening. Today there are more options for these patients, and this guide provides knowledge, navigation and support.
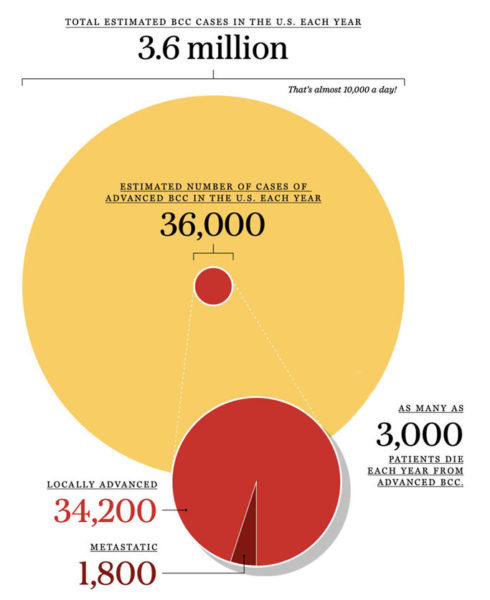
One of the toughest things a doctor ever has to do is deliver a cancer diagnosis — but dermatologists do it every day. Skin cancer is common; in fact, basal cell carcinoma (BCC) is the world’s most common cancer, so dermatologists see a lot of it. While it is difficult to pinpoint the exact number of BCC cases in the U.S., The Skin Cancer Foundation estimates it as 3.6 million a year. That’s nearly 10,000 diagnoses a day.
Some BCC Basics
- BCCs are uncontrolled growths that arise from basal cells in the outermost layer of the skin. Most BCCs are caused by exposure to ultraviolet (UV) radiation from the sun. UV from indoor tanning can also increase risk for BCC.
- Over time, UV radiation damages DNA in the skin. The body repairs some of the damage, but what remains unrepaired can trigger mutations that lead to skin cancer.
- Not all BCCs look alike. In fact, they might look like a pimple, a sore that doesn’t heal, a shiny bump, a scar-like area, a pink or reddish patch or something else. In patients with darker skin, about half of BCCs are pigmented (meaning brown in color). Some people develop multiple BCCs over a lifetime.
- The good news: Because skin cancer is a cancer you can see, these tumors tend to be detected early, when they are easiest to treat and have the best chance of a cure. The Skin Cancer Foundation’s Big See campaign keeps it simple: Look for anything new, changing or unusual on your skin and let your dermatologist know. With early detection and prompt treatment, almost all BCCs can be successfully cured without complications.
- The not-so-good news: There are some exceptions. “It’s essential for people to understand that in its advanced stages, BCC can be disfiguring and even deadly if left untreated, just like any other cancer,” says John Strasswimmer, MD, PhD, a board-certified dermatologist based in Palm Beach County, Florida, who focuses on Mohs surgery and cutaneous oncology. “We’re just lucky that we have become good at diagnosing and treating it most of the time.”
Below the Surface
BCCs are notorious for often looking like “no big deal” on the surface while growing “roots” that can burrow deep into the skin and cause damage. Like rogue tree roots that burrow into the ground and disrupt underground plumbing, cable and utility services, BCCs can invade deep into the skin and even damage nerves, muscle and bone.
“What we see with BCC on the outside may not always be what is present on the inside,” Dr. Strasswimmer explains. There are several reasons for this. Sometimes it is just the way the cancer grows. Other times it may be due to a previous treatment that didn’t remove the entire tumor. While researchers are looking into new ways of imaging that may eventually help dermatologists see what is under the skin, for now there is no crystal ball.
Luckily, though, there is Mohs surgery. This gold standard technique allows a specially trained surgeon to remove a layer of tissue at a time, examine the tissue under a microscope in an adjacent lab, identify exactly if and where any remaining cancerous cells are located and repeat the process until no microscopic cancer cells remain. The surgeon examines nearly 100 percent of the tumor margins, spares healthy tissue and leaves the smallest scar possible.

Focus on Mohs Surgery. Dr. Strasswimmer started his practice in Southeast Florida in 2005 to fill a need for specialized care for patients with advanced skin cancer. Photo: John Strasswimmer, MD, PhD
Dr. Strasswimmer recalls a patient with a very small BCC on the side of her nose that looked like a small red patch or a pimple. “When I did my first Mohs surgery layer removal, I could see that the tumor was going quite deep. By the time I got the tumor out, it was down to the bone. We had to remove the outer layer of the bone and then do some reconstruction.”
He later learned that previously the patient’s BCC had been burned off superficially by an electrolysis device for hair removal. “That removed the visible part on the surface but did not remove the whole tumor and thus allowed cancerous cells to proliferate underneath and cause a tremendous amount of devastation,” Dr. Strasswimmer says. Some people have used DIY devices and home remedies they read about to remove a lesion or mole from their skin. This is a dangerous practice that can make early detection and treatment of skin cancers such as BCCs much more difficult.
What Is Advanced BCC?
Remember, the majority of BCCs are caught early. Some very early lesions may be treated with minimally invasive options such as topical treatments, curettage and electrodesiccation, cryotherapy or laser surgery. Others may be treated with excisional surgery, Mohs surgery or radiation. (See the SCF Treatment Glossary for more information.)
However, a small proportion of tumors can become advanced and penetrate deep into the skin and surrounding tissues (locally advanced) or spread to other parts of the body (metastatic). Treatment for advanced BCC may include surgery, radiation or systemic medications, which treat the cancer from inside the body.
How do BCCs become advanced? In many cases, patients with advanced BCC have had previous treatment or multiple treatments, but the cancer has recurred or spread, says Lara A. Dunn, MD, a medical oncologist at Memorial Sloan Kettering Cancer Center in New York City.

Early Detection Is the Key! Postponing a dermatologist visit, says Dr. Strasswimmer, may allow small BCC tumors to grow and become advanced. Photo: John Strasswimmer, MD, PhD
In other cases, it is simply due to “benign neglect,” Dr. Strasswimmer says. There are lots of reasons for this, including fear of what a lesion might be, fear of what the treatment might entail or worries about medical costs or lack of insurance. He has seen many patients in his practice with advanced BCC who were diagnosed years earlier and left untreated.
“In some cases, BCCs may not be that uncomfortable,” he adds. “Patients may keep a lesion hidden from loved ones and procrastinate on seeing a doctor about it until it grows very large. People underestimate how cost-effective in-office surgery can be, which likely could have cured the BCC if treated early. Many patients have postponed seeing their dermatologist during this long pandemic, and that’s understandable. But it also can be costly — in more ways than one.”
There are two categories of advanced BCC: locally advanced and metastatic.
Locally Advanced BCC: The definition of locally advanced BCC generally includes several types of presentations: large, deep, aggressive tumors; those that have recurred after treatment; and cases where surgery or radiation would not be effective or appropriate.
“After a previous treatment, the BCC may have recurred in the area where it started, or in the surrounding area, and caused extensive damage to surrounding tissue, muscle, bone or nerves,” says Dr. Dunn. “Or it could have traveled through the regional lymphatic system into the lymph node nearest where the tumor originated.”
Some patients with locally advanced BCC have already been treated with multiple surgeries and radiation, she explains, which can make it almost impossible to get clear results with another surgery. Or, the tissue may have already been exposed to the maximum amount of radiation it can receive. Dr. Strasswimmer stresses the importance of seeing a board-certified radiation oncologist.
Dr. Dunn says there are also cases in which these tumors are neglected and have become so large that an initial surgery is not an option or would be so extensive that it would greatly affect function, such as removal of the eye, she explains. “In those situations, we might be able to try radiation.”
Metastatic BCC: Far less common than locally advanced, metastatic BCC is when the cancer has “broken loose,” as Dr. Strasswimmer describes it, and spreads to a distant lymph node or to another organ in the body, such as the lungs, or sometimes to another area in the skin. About 70 percent of total metastatic cases spread through the lymphatic system, but they can also spread through the bloodstream or under the skin.
How Many People Develop Advanced BCC?
Because nonmelanoma skin cancer is not tracked by cancer registries in the U.S., it is difficult to pinpoint the number of BCC cases, let alone advanced BCCs. Studies have suggested that a range of 1 to 10 percent of total cases of BCC become advanced. The Skin Cancer Foundation uses the conservative estimate of 1 percent. Of those, 95 percent are estimated as locally advanced and about 5 percent are metastatic.
Systemic Treatments for Advanced BCC
Seeing patients with advanced BCC earlier in his career “was a heartbreaking time,” Dr. Strasswimmer remembers, “because we had patients then who could not be treated. Surgery and radiation were no longer options. All we could do was to provide comfort and keep their symptoms as controlled as possible.”
Today there are newer options for these patients. For some advanced cases, patients may receive a type of medicine taken orally called hedgehog inhibitors, or HHIs. This medication works by blocking abnormal signals that promote cancerous growth. “However, if a patient develops a tumor that is resistant to these medications or has not tolerated them due to side effects, there hasn’t always been a standard backup option for them,” says Dr. Strasswimmer.
Immunotherapy is another systemic treatment option that has been helping patients with many types of advanced cancers in recent years. Immunotherapy works by using the body’s own immune system to help attack cancer cells. Intravenously infused immunotherapy medications called checkpoint inhibitors work by blocking a protein receptor called PD-1 (programmed death-1), which, under normal circumstances, helps keep the immune system in check. These drugs release T cells to fight the cancer.
Research is rapidly progressing, and keeping up with the latest advancements can make all the difference for patients. Dr. Dunn says she is hopeful that emerging therapies will provide additional options for her advanced BCC patients.
Dr. Strasswimmer is also encouraged by recent developments in the treatment of advanced BCC and the impact it could have on his patients.

Regeneron and Sanofi financially supported and collaborated in the development of this article with The Skin Cancer Foundation.
ONC.21.020031 04/2021




 Patients with any advanced cancer can benefit from
Patients with any advanced cancer can benefit from 
